At Kaki Prod, we’ve got a thing for healthcare systems—spotting the differences around the globe is like our jam. Our analysis takes a deep dive into these setups, zooming in on the big three: accessibility, quality, and cost.
We’re gonna dig into the strengths—and yep, the weaknesses too—of different models. That means the U.S. system gets the spotlight, plus those universal healthcare options in places like the UK, Canada, France, and Japan.
This whole shebang isn’t just for kicks. It’s about uncovering insights into what nails it… and what falls flat, helping us piece together the puzzle of where global healthcare is headed.
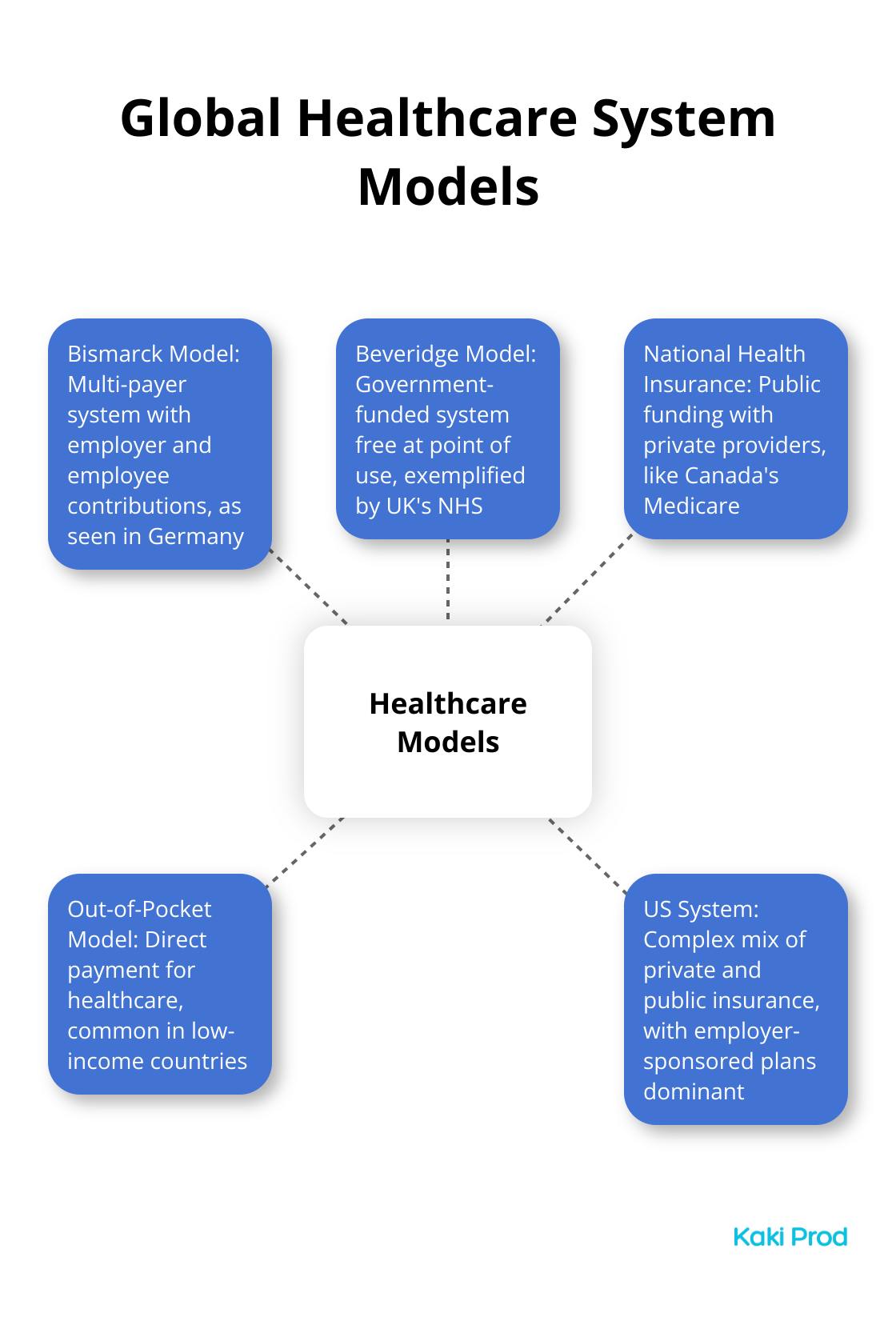
Global Healthcare Models Compared
The Bismarck Model: Germany’s Approach
Germany rolls out the red carpet with its Bismarck model, a healthcare veteran on the European stage. This multi-payer system ropes in employers and employees to chip in for sickness funds. It’s a win-win – universal coverage without blowing the budget. Health spending in Germany is a triple-threat measured in GDP percentage, health spending percentage, and USD per person (yeah, it’s all here in black and white).
The Beveridge Model: UK’s National Health Service
Ah, the UK and its NHS – a poster child for the Beveridge model. Think of it like healthcare’s all-you-can-eat buffet, courtesy of Her Majesty’s government and funded by taxes. Free at the point of need for anyone with a UK address. But (and there’s always a but), the queues can be like waiting for Christmas…next year. They keep tabs on wait times for Consultant-led Referral To Treatment (RTT), giving you the lowdown from doc’s note to treatment day (check it out).
The National Health Insurance Model: Canada’s Medicare
Canada’s giving a masterclass with its National Health Insurance model – Medicare. Public purse, private providers. It’s inclusive, yet those wait times? Like watching paint dry. A 2022 report says Canadians were on standby for a median of 27.4 weeks between a GP’s nod and actual treatment.
The Out-of-Pocket Model: A Global Challenge
Let’s zoom in on cash-on-the-barrelhead healthcare – alive and kicking in many low-income nations. Talk about a recipe for health inequality. The World Health Organization drops a bombshell stating healthcare costs plunge 100 million folks into deep poverty every year (WHO, 2023), which is – let’s be honest – insane.
Top-Ranked Healthcare Systems
Now, the rockstars of health: Taiwan, South Korea, and Japan. CEOWORLD magazine crowned these as the healthcare titans in 2021. They’ve nailed universal coverage with slick service delivery and cutting-edge tech (see it to believe it). As we hop on the AI train in healthcare, it’s all about forecasting health hiccups and catching them early to flex those tech muscles.
Dive into the healthcare rabbit hole before packing up and moving countries. Every system has its bag of tricks and troubles impacting care access, service quality, and overall health vibes. Next on the docket: the American healthcare saga, a tale that – spoiler alert – goes against the grain of most worldwide systems.
The US Healthcare System: A Complex Tapestry
A Unique Blend of Public and Private Coverage
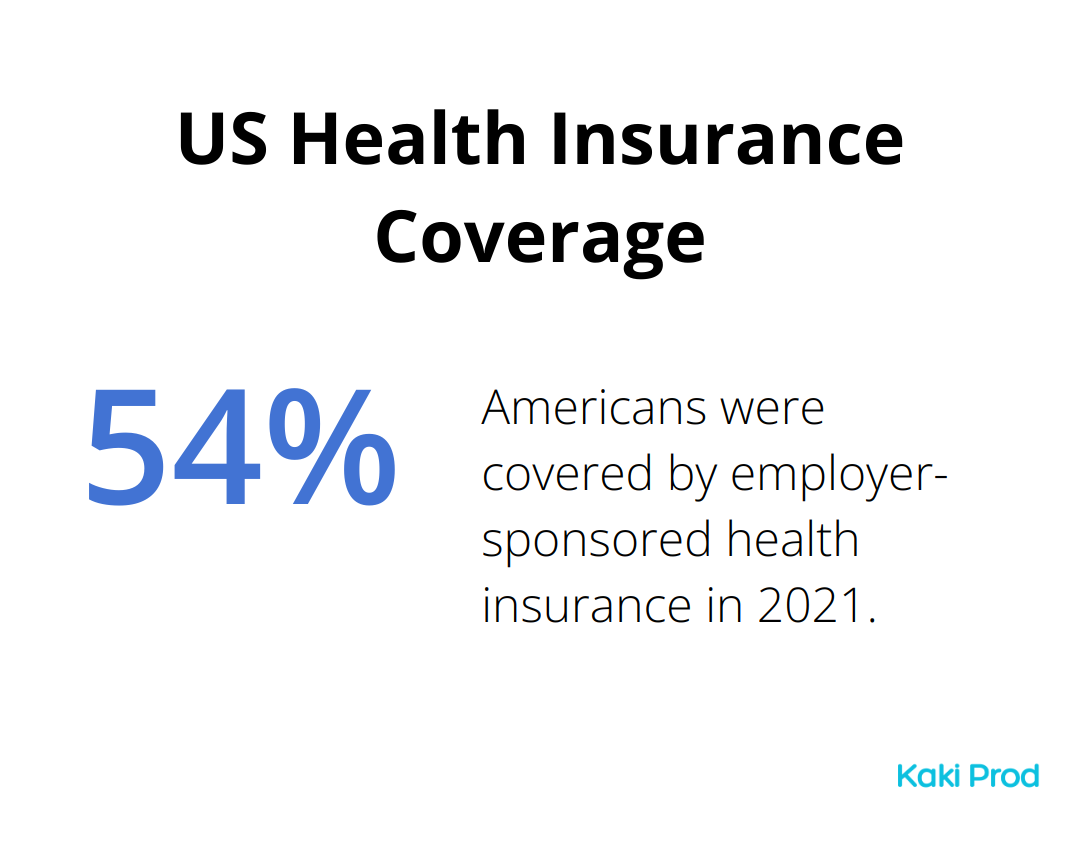
Ah, the US healthcare system… a maze of epic proportions. Unlike its peers abroad, it’s a cocktail of private and public insurance. You’ve got Medicare (the lifeline for those 65 and wiser) and Medicaid (the safety net for those tighter on cash). The rest? Well, they’re navigating employer-sponsored plans like a map with no compass. In 2021, a cool 54.4% of Americans were in the employer camp (thanks, Kaiser Family Foundation, for the stats).
And for the rest without employer goodies? The ACA marketplace awaits-though, spoiler alert: 8.6% are still dodging the insurance bullet, risking those jaw-dropping medical bills we all love.
Cutting-Edge Care at Premium Prices
The US system-glitzy with its high-tech, cutting-edge medical wizardry. The leader of the medical research pack, thanks to National Institutes of Health, splashing out $47.7 billion for 2024. All that dough brings bleeding-edge treatments straight to America’s doorstep.
But let’s be real… those innovations don’t come cheap. The US has turned healthcare spending into an extreme sport.
Navigating the Insurance Labyrinth
If you’re new to this insurance jungle, brace yourself. Plans all over the place-coverage and costs that make your head spin. Here’s the quick and dirty lowdown:
- Premiums: Fork it over monthly or watch the coverage ghost you.
- Deductibles: The cash barrier you leap over before insurance shows up.
- Copayments: Set amounts for this, that, and the other.
- Out-of-pocket maximum: The ceiling on what you’ll pay each year.
A 2021 survey (shout-out to Kaiser Family Foundation) pegged the average price tag for employer-sponsored family coverage at $22,221, with workers chipping in around $5,969. A steal, right?
But wait, there’s more! The basics are just the beginning-step into the world of in-network vs. out-of-network, pre-authorization head-scratchers, and coverage quirks that even baffle seasoned insurance warriors.
The Impact on Patient Care
How does this epic maze of a system hit patients? It’s a mixed bag. Sure, you’ve got laser-precision specialists and the latest medical tech. But many folks hit pause on care or skip it altogether due to costs. A 2022 Gallup poll found 38% of Americans had to slam the brakes on medical treatments, their budgets crying for mercy.
It’s quite the contrast from other developed nations, where universal coverage breeds healthier populations without blowing the budget.
As we dive deeper into the global healthcare scene, particularly universal systems, the US’s kaleidoscope of complexity offers a lens into the myriad ways countries tackle the healthcare conundrum. Buckle up-it’s a wild ride.
Universal Healthcare Models Worldwide
UK’s NHS: Free at the Point of Use
The National Health Service (NHS) in the UK is your all-access pass to healthcare-not a penny at the point of use. We’re talking tax-funded magic that covers everything from the sniffles to big-league surgeries. But here’s the kicker-the NHS is in a bit of hot water. Think waiting times that could test the patience of a saint, as today’s headlines in the UK will tell you.
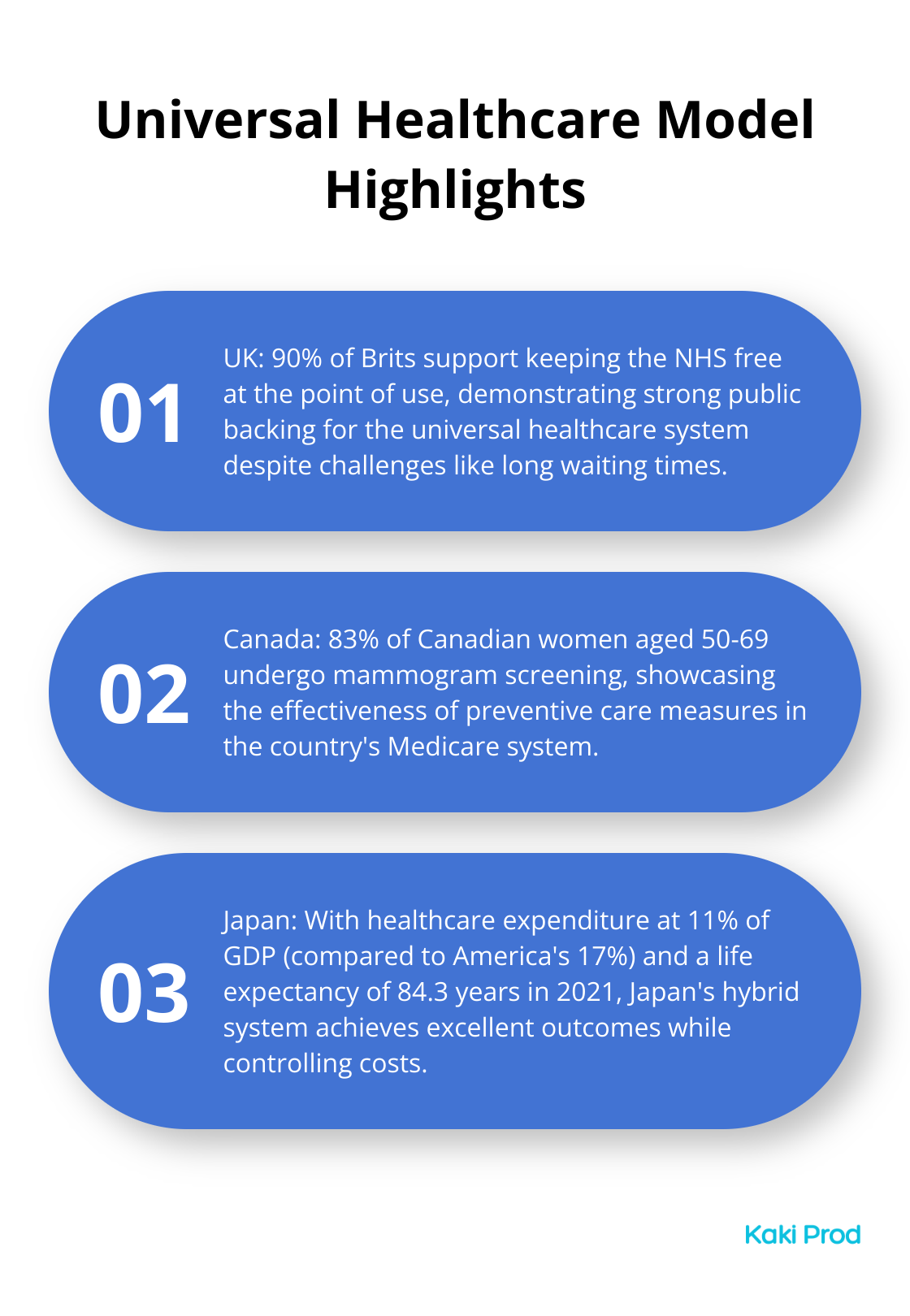
Yet, the NHS is still the darling of the public. A 2023 survey gives it a glowing review: 90% of Brits say, “Keep it free at the door.”
Canada’s Medicare: Provincial Power
Welcome to Canada’s multi-layered healthcare world. It’s like healthcare on a buffet line-individual institutions, health regions, and entire provincial systems. The provinces call the shots while the federal government sets the stage and hands over the cash.
Canada’s shining light? Preventive care. They’re the overachievers in cancer screening-83% of women aged 50-69 ticking that mammogram box, says Statistics Canada.
France’s Statutory Health Insurance: Public-Private Partnership
Over in France, it’s a healthcare mash-up extravaganza. France’s system? It’s a combo platter of universal coverage with public and private providers shaking hands. The whole setup is like a health safety net woven with principles-coverage, solidarity, accessibility, you name it.
France’s report card? Stellar health stats, ranking up there in life expectancy-82.3 years in 2021 if you’re keeping score (thanks, World Bank). Low rates of preventable deaths too (133 per 100,000 in 2019, thanks, Eurostat).
But picture this-financial clouds on the horizon. In 2022, their deficit peaked at €18.9 billion, sparking furious coffee-fueled debates about what’s next.
Japan’s Hybrid System: Employer-Based Coverage
Then there’s Japan, taking a page out of a hybrid healthcare playbook. Here, everybody’s got insurance-either via an employer or a government gig. This setup nails universal coverage while keeping a tight budget.
Japan’s healthcare tab? Just 11% of GDP, a steal compared to America’s 17% (hat tip, OECD). And what do they get for it? Top-tier health outcomes like leading the world with life expectancy-84.3 years in 2021.
Still, challenges loom large. An aging crowd is putting the squeeze on resources, and there’s a healthcare worker shuffle with a 130,000 nurse shortfall reported in 2022 by the Japan Medical Association.
These snapshots are like a VIP tour through universal healthcare’s wonders and woes. Each one with its own flavor of strengths and hurdles, all trying to strike the balance between access, quality, and the almighty dollar.
Final Thoughts
Healthcare systems around the world – it’s like a global buffet of options, from universal coverage to pay-as-you-go. Sure, everyone loves better outcomes and less cash bleed with universal coverage, but… yeah, brace for the line. The U.S.? An innovator’s dream with all the shiny tech, but if you’re not rolling in dough, well… good luck finding the care you need.
So, what’s brewing on the horizon? Digital – that’s what. AI is slipping on its white coat, and telemedicine is the new house call. Prevention? It’s now in vogue, along with tackling those sneaky social factors that play havoc with health. Oh, and let’s not forget – economies are graying faster than your grandparents. This shift will throw down the gauntlet to healthcare systems, demanding they get creative to keep the care quality up without the costs running wild.
Here at Kaki Prod, consider us your backstage pass to this healthcare opera, and more. With our EverydayNext platform, we’ve got your back as you chart a course through this ever-evolving play. Whether it’s snagging the best health tips or leveling up your career, we’re here to supercharge your journey toward a future that’s… well, better.

